Improving API Solubility
Read more about
- The Importance of API Solubility for Solid and Liquid Dosage Forms
- The Solubilization Process
- The Biopharmaceutics Classification System of APIs
- The Developability Classification System
- The Central Role of Solubility and Permeability for API Absorption
- Strategies for Enhancing API Solubility
- A Path for Addressing API Solubility Challenges
- The Value of a Trusted Partner
The Importance of API Solubility for Solid and Liquid Dosage Forms
A sufficient level of solubility is critical to the efficacy of small molecule drugs – whether in a solid or liquid dosage form.1 In oral administration, the active pharmaceutical ingredient (API) must be absorbed by the body to become bioavailable and enter the systemic circulation to deliver the intended physiological effect. Poor solubility on the other hand results in low absorption from the gastrointestinal (GI) tract, with the API potentially not reaching therapeutic levels at the site of action. For parenteral formulations, good API solubility is critical as well as a prerequisite for particle free solutions and can be even more challenging in the case of high concentrated formulations. If an API that is orally administered via a solid dosage form does not fully or just partly dissolves within GI fluids, it cannot permeate through the intestinal membrane and does not achieve the desired therapeutic effect. Many APIs that are currently on the market suffer from poor solubility. However, this challenge will become increasingly important as up to 90% of all drugs in the small molecule development pipeline are estimated to be poorly soluble. If this problem cannot be addressed, a promising medication may never make it to the market.2
The Solubilization Process
High lipophilicity and strong intermolecular forces impact solubilization of drug molecules.1 Solubility is the ability of a solute to dissolve in a solvent, forming a homogenous mixture. The process of solvation can be broken down into three steps as diagrammed in Figure 1.
- A solute molecule must be separated from the solid state by breaking solute-solute bonds.
- A gap must be created within the solvent.
- The solute molecule must be incorporated within the solvent.

Figure 1.1A single molecule is removed from the crystal lattice: crystal packing energy.
Figure 1.2A gap is created in the solvent: cavitation energy.

Figure 1.3Thesoute inserts in to the solvent: solvation energy.
Figure 1. The process of solubilization
Equilibrium solubility is defined as the point at which the dissolution rate is equal to the precipitation rate and is the maximum amount of substance that can be dissolved in a stable equilibrium.
The measure of equilibrium is a thermodynamic value and does not take into account the rate at which the system reaches equilibrium. Because of this, such measurements can be misleading, If a compound has acceptable equilibrium solubility but also a poor dissolution rate, the compound may not reach the expected concentration levels in the GI tract before being cleared out of the body. In this situation, absorption may not reach the desired level.
Figure 2 shows the process of dissolution. For a drug particle to dissolve, a concentration gradient must be present between the drug in free solution (C) and the drug concentration on the surface of the dissolving solid (Cs), separated by a layer of unstirred solvent (h).
This gradient allows diffusion of the solid that is in the process of dissolving through the unstirred layer and into solution. The rate of dissolution is thus equal to the rate of diffusion through the unstirred solvent layer.
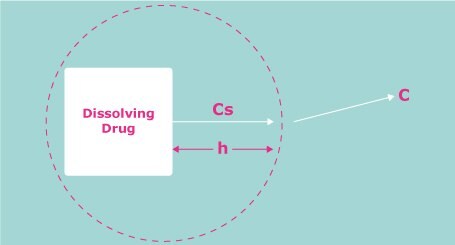
Figure 2.The process of dissolution. A drug molecule must break from the solid bulk and dissolve through the unstirred water boundary, h, before passing into solution.
The Biopharmaceutics Classification System of APIs
The importance of API solubility is reflected in the Biopharmaceutics Classification System (BCS). Developed in the 1990s, the BCS categorizes APIs in terms of their solubility and permeability and correlates this with their potential in vivo performance (Figure 3).3 The system was originally used by the United States Food and Drug Administration (FDA) as the basis for biowaiver applications.
As defined by the BCS, Class I molecules exhibit good solubility and good permeability, and are expected to have good absorption in the GI tract. BCS Class II compounds have low solubility and high permeability, while BCS Class III molecules have high solubility and low permeability. The most challenging class of molecules have low solubility and low permeability and are categorized as BCS Class IV. Approximately 30-40% of all marketed drugs have low solubility (BCS Class II and IV).2
As high throughput screening and target-oriented drug discovery often result in poorly water-soluble APIs, the percentage of drugs and drug substances with this shortcoming is expected to increase. With an estimated 70–90% of drugs currently under development being poorly soluble, new strategies are needed to overcome this challenge (Figure 4).2

Figure 3.The Biopharmaceutics Classification System categorizes APIs in terms of permeability and solubility into four classes.
Distribution of marketed |
Distribution of drug substances in the pipeline |
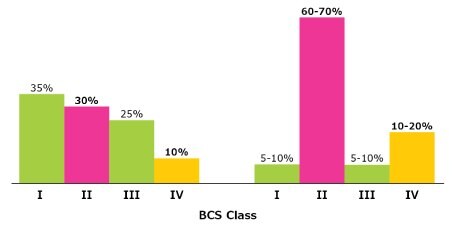
Figure 4.Marketed drugs and drug substances in the pipeline classified by the BCS.
The Developability Classification System
The BCS served as a basis for the Developability Classification System (DCS).4 The DCS added a solubility-limited absorbable dose (SLAD) line to further differentiate APIs within Class II (Figure 4). Drugs above the SLAD line are dissolution rate limited (DCS Class IIa), while those below are solubility limited (DCS Class IIb). Solubility is tested using biorelevant FASSIF (fasted state simulated intestinal fluid) media, providing a more accurate reflection of what is taking place in the human body. This allows formulation scientists to be less conservative and to shift the dose solubility ratio from 250 to 500.
Overall, the DCS allows formulation scientists to understand the root causes of a solubility challenge and distinguish between the two classes, providing important insights to guide efforts to address the problem.

Figure 5.The Developability Classification System for APIs adds to the Biopharmaceutics Classification System by including Class IIa for dissolution rate limited APIs and Class IIb for solubility limited APIs.
The DCS categorizes APIs based on the factor responsible for poor absorption:
- Dissolution rate-limited: The dissolution rate is too slow for the API to dissolve during time of passage by the site of absorption (usually the small intestine).
- Solubility-limited: The solubility is too low for the required amount of API to dissolve in the available GI fluid volume.
- Permeability-limited: The rate of transfer from GI tract through the intestinal membrane is too low. There is limited influence on permeability by excipients choice and formulation.
The Central Role of Solubility and Permeability for API Absorption
LADME, an acronym that stands for liberation, absorption, distribution, metabolism, and excretion, summarizes the criteria that influence drug levels, the kinetics of exposure, and ultimately, the pharmacological activity of a drug (Figure 5). This model reinforces the central role of solubility and permeability for proper absorption of an API from the intestinal tract into the circulation. Absorption of an API can be increased using chemical and physical approaches to enhance solubility, while permeability can be improved using enhancers, increasing API lipophilicity, and altering the route of administration.

Figure 6.Overview of different approaches used to improve API bioavailability including those for solubility and permeability enhancement.
Strategies for Enhancing API Solubility
A number of techniques can be applied to enhance the solubility of APIs based on their DCS categorization (Figure 6).
For APIs that are dissolution-rate limited (DCS IIa), physical modification in the form of particle size reduction by micronization and nano-milling can be used. This challenge can also be addressed with strategies to promote dissolution including disintegration acceleration, dissolution enhancers, and by replacing hydrophobic lubricants with hydrophilic lubricants. While lubricants are only relevant for solid dose formulations, disintegration accelerating approaches and dissolution enhancers are strategies relevant for both liquid and solid final dosage forms.
Strategies that can be used with solubility limited APIs (DCS IIb) include chemical modification via API processing and different enabling formulation approaches. Chemical modification includes polymorph screening, salt formation, cocrystal formation, and prodrug formation and can be applied regardless of the final dosage form. Formulation-based approaches include solid dispersion technologies such as hot-melt extrusion, spray drying, and drug carrier systems which are mainly relevant for solid dosage forms. API complexation with cyclodextrins can be used to improve both API solubility and stability in liquid, semi-solid, and solid formulations.
Additional approaches to enhance solubility include the use of surfactants and the usage of in-situ counter-ions like meglumine, which are suitable for liquid, semi-solid, and solid final dosage forms.

Figure 7.Strategies and enabling technologies for enhancing API solubility of dissolution rate and solubility limited APIs.
A Path for Addressing API Solubility Challenges
The number of drugs in development with solubility limitations, which can potentially be addressed via formulation, will continue to increase. Fortunately, there are many options for overcoming this challenge. Once the underlying cause of an API solubility issue is identified, application of the proper solution can result in the enhancement needed to help deliver the intended therapeutic effect.
The Value of a Trusted Partner
Selecting the best formulation strategy to address the specific challenges presented by different APIs can be time-consuming and complex. Prior to arriving at the final formulation, many obstacles must be overcome and may include API stability, bioavailability, and release kinetics, just to name a few.
Finding a trusted partner with expertise in applications and regulation can help identify the best approach for your specific API, solve a range of solubility challenges, and accelerate development timelines. We offer comprehensive formulation support and solutions for the development of customized oral dosage forms through our Application Services. With our broad R&D expertise, we offer application know-how, an extensive portfolio of innovative excipients, and the technologies you need for formulation success.
For more detailed information on strategies for enhancing API solubility:
- Read about the various methods for API processing, tackling API solubility early during development
- Read about dissolution enhancement methods to help you decide between the many options to take during formulation
- Read how Hot Melt Extrusion with polyvinyl alcohol (PVA) is used to enhance API solubility
References
To continue reading please sign in or create an account.
Don't Have An Account?